Low Sodium: Not Just Your Mom’s Cooking
Case Information:
Mr. D is a 42-year-old man who is brought to the emergency department by the police department. He is disoriented and confused. Initial labs reveal a serum sodium concentration of 118 mEq/L.
Due to his confusion, Mr. D cannot give a medical history. His chart is requested. Physical exam reveals a disheveled man appearing older than 42. He smells of alcohol. His vital signs are BP, 90/50 mm Hg; pulse, 90 bpm; temperature, 36.0°C; RR, 18 breaths per minute. He has no orthostatic changes. Neck veins are flat. His lungs are clear to auscultation. Cardiac exam reveals a regular rate and rhythm. There is no jugular venous distention (JVD), S3 gallop, or murmur. His abdomen is distended, and his flanks are bulging. Extremity exam reveals 3+ pitting edema extending all the way up his thighs.
Laboratory studies reveal a glucose of 100 mg/dL, K+ 3.8 mEq/L, a BUN of 28 mg/dL, creatinine 1.0 mg/dL, and a serum osmolality of 252 mOsm/L. Urine osmolality is 480 mOsm/L.
Review of Mr. D’s past medical record reveals that he has a long history of alcohol-related complications. Six months ago, he was hospitalized for bleeding esophageal varices.
Lab studies reveal an albumin of 2.1 g/dL, bilirubin 6.2 mg/dL, AST (SGOT) 85 units/L, ALT (SGPT) 45 units/L, INR of 1.8. An abdominal ultrasound reveals moderate ascites and a small liver with coarse architecture suggestive of cirrhosis.
An echocardiogram reveals normal left ventricular function and a urinalysis reveals only 1+ proteinuria not suggestive of nephrotic syndrome. A paracentesis is performed to rule out spontaneous bacterial peritonitis and is normal.
Mr. D’s mild hyponatremia is corrected slowly. He is begun on free water restriction and his sodium gradually improves to 128 mEq/L. His mental status returns to normal.
S: 42 y/o disoriented, and confused man with a past history of alcohol-related complications and esophageal varices who smells of alcohol is brought to the emergency department with a 3+ pitting edema extending to his upper legs. Pt also presents with abdominal distention and flank bulging. Pt cannot provide medical history due to altered mental state.
O: BP 90/50, P 90 beats/min, RR 18 breaths/min, T 36.0°C.
Cardiovascular exam: Neck veins flat. Regular rate and rhythm. No jugular venous distention (JVD), S3 gallop, or murmur.
Pulmonary exam: Lungs clear to auscultation.
Abdominal exam: Abdomen distended and bulging flanks.
Extremity exam: 3+ pitting edema extending all the way up the thighs
Initial serum sodium concentration of 118 mEq/L. Normal glucose (100 mg/dL), K+ (3.8 mEq/L), creatinine (1.0 mg/dL), and urine osmolality (480 mOsm/L). Elevated BUN (28 mg/dL). Decreased serum osmolality (252 mOsm/L). Albumin of 2.1 g/dL, bilirubin 6.2 mg/dL, AST (SGOT) 85 units/L, ALT (SGPT) 45 units/L, INR of 1.8.
Abdominal ultrasound: moderate ascites and a small liver with coarse architecture suggestive of cirrhosis.
Echocardiogram: normal left ventricular function
Urinalysis: 1+ proteinuria – not indicative of nephrotic syndrome
Paracentesis: normal
Improved serum sodium concentration (128 mEq/L) following free water intake.
A: Hypervolemic hyponatremia secondary to cirrhosis
Heart failure and hyponatremia
Nephrotic syndrome
P: Slow correction of hyponatremia — Free water restriction
Summary:
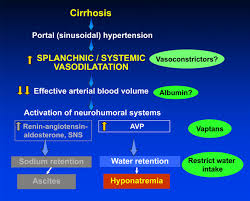
Hyponatremia is a condition characterized by low serum sodium levels. Since Mr. D smells very strongly of alcohol and is also hyponatremic and hypervolemic as per his initial serum sodium measurement and edema, respectively, it is most likely that he suffered from cirrhosis. This is further supported by his bulging flanks and abdominal ultrasound findings of ascites and other liver abnormalities.
Nephrotic syndrome is initially considered as an alternative diagnosis as a result of Mr. D’s hypoalbuminemia, edema, and hypervolemia. However, nephrotic syndrome is ultimately ruled out as a result of the lack of increased proteinuria as reported by the results of the urinalysis.
In treating Mr. D’s hyponatremia as a result of cirrhosis, a slow approach is taken because of his current condition and other context clues. While Mr. D is confused and disoriented, he does not seem to have any severe neurological symptoms that would warrant a rapid return to normal serum sodium levels. His mental state returned to his normal following slower water restriction. Additionally, the context of his chronic liver disease as a result of alcohol abuse points to the idea that fast correction of the hyponatremia would increase Mr. D’s risk of osmotic demyelination syndrome, which could be fatal. Thus, the safest solution for Mr. D was a gradual return to a normal serum sodium level.